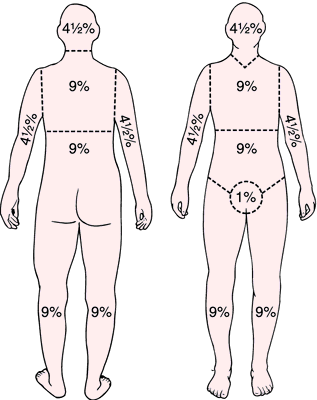
"Rule of Nines"
It is a method of estimating the extent of burns, expressed as a percentage of total body surface. In this method, the body is divided into sections of 9 per cent, or multiples of 9 per cent, each: head and neck, 9 per cent; anterior trunk, 18 per cent; posterior trunk, 18 per cent; upper limbs, 18 per cent; lower limbs, 36 per cent; genitalia and perineum, 1 per cent. The rule of nines is fairly accurate for adults but does not allow for differences in proportion in children, for whom the lund and browder classification is generally used.